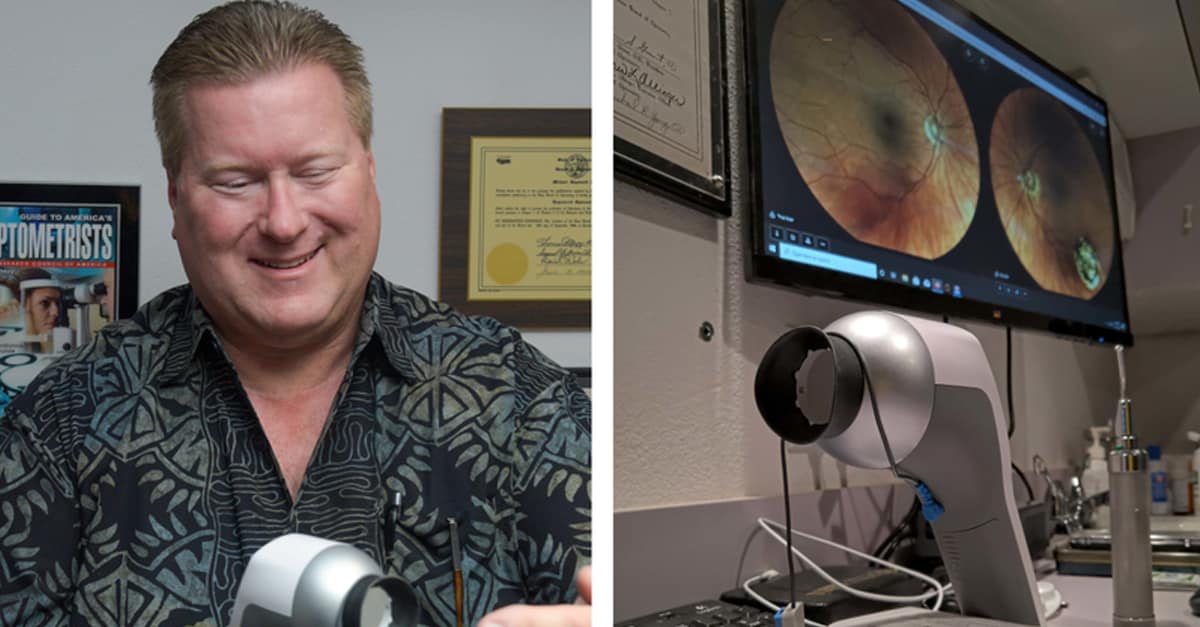
Optometrist Michael Young Re-Discovers RETeval
A Vision from the Past…
Deciding to take in a class while attending a vision conference, Redding optometrist Michael Young expected to receive new knowledge, but he was not ready for the impact that came with it. The trigger was mention of a new high-tech instrument for detecting vision disorders. And though Young had never seen this gadget before, his jolt was one of recognition.
Because, as an undergrad research assistant working with a team at Pacific University School of Optometry some 30 years ago, he had helped gather and analyze data, developing the basic science that led to the manufacture of the device being described to him in 2018.
“It’s basically utilizing the research we did back in the ‘80s,” he says in his office a year later. “It was a ‘wow’ moment. It’s not every day you see something come to fruition that you participated in.” After that class, he headed straight for the convention floor to check one out.
Today the RETeval, made by LKC Technologies, boasts a history of clinical trials and eye doctors’ praise of its performance. It’s been called fast and accurate in detecting early signs of diabetic retinopathy, sight-threatening diabetic retinopathy and glaucoma. Early detection, it is widely believed, can mean slowing – or prevention – of optic nerve damage.
Redding optometrist Ken Ekelund seems impressed with his RETeval. “It measures light going into the photoreceptors of the eye, the rods and cones. We’re looking for the electrophysiological response time,” he explains. “It’s sort of like an EKG for the eye. Tests like this used to take an hour. Now it’s more like 60 seconds.”
And, of course, Young bought one. “They packed everything into it that they could,” he says, aiming at his cupped hand a device the size and shape of a hand-held hair dryer. “It has 38 different test protocols. All analysis is done by the instrument. Then you can plug into a computer for storage and printing.”
He was shocked to see something so portable and easy to use, in stark contrast to the equipment they used back in that college lab. “It takes the place of a computer in 1988 that would fill a room,” he marvels. “That kind of equipment didn’t have a practical application in a clinic. We used to do everything by hand. We used to pull the graphs and hand-analyze the data.”
The team with which undergrad Young worked collected and analyzed variations in retinal response time. “It was to better understand the visual system in the brain, and visual response to stimulus,” he says. “My role was to gather data and run tests on the subjects.”
Government grants funded the research, which included law enforcement and the U.S. Air Force. For the former, the team first had to get their test subject drunk. “We liquored them up from 0.08 to 0.15,” Young recalls. “Predictably, we saw increased latency in the strength of the signal. Their response time was wrecked.”
Their Air Force work proved to be a bit more interesting. A 1983 copy of a progress report to the grantor by the team’s leader, Dr. Robert Yolton, describes visual response tests on subjects from the general public, evaluating for the degree of variability of response while employing a set of specific factors.
Hooray for science, right?
But things had changed by the time undergrad Young joined the team, two years later. Then they focused testing on Air Force pilots, employed a specific factor of G-force and analyzed the variability of response times between a pilot facing a friendly object and that same pilot facing one of an enemy.
“They wanted to arm weapons with a pilot’s brain,” says Young. “They wanted to automate a system based on a pilot’s recognition. It didn’t work. We couldn’t find a clear differential in response between friend or foe.”
Young arrived in Redding from Eureka at the tender age of 6 weeks and, except for some time away for college, has been here ever since. He never saw an eye doctor as a youth until he tried for his learner’s permit at the DMV and failed. “I was 15 and a half when I got my first pair of glasses,” he remembers. “It was so eye-opening to see the feast. Right then I knew this is what I wanted to do for other people.”
At Pacific University College of Optometry, just up a state in Forest Grove, Ore., Young learned that his probable professor, Yolton, headed a research program. “I applied for a paid position in the lab before taking the class,” Young says. “I basically learned everything I needed in the research lab. Class was easy after that.” He graduated second in his class.
For about a year now, Dr. Michael Young has been aiming his RETeval into his patients’ eyes. “With glaucoma or anything that damages the optic nerve, we can see a change in the response time,” he says. On the device he helped spawn, he adds, “I don’t know how to improve it. I utilize only part of it now, maybe 10 percent. I would like to learn how to utilize it more.”
After being so dramatically reminded how far technology has reached into his profession, Young is ready for further evolution. “I think it’s going to make things easier,” he muses. “What would be really helpful would be gene-type therapy for macular degeneration, and possibly optic nerve repair. Who knows what the future will bring? Thirty years ago, an optometrist could screen and refer. Now we can screen and treat.”
His smile carries a certain pride. •
Michael R. Young, OD • 841 Hartnell Ave., Redding(530) 222-1233 • www.reddingeyecareca.com